When I was training as a play therapist, one of the first exercises we did was a task to enable us to begin to understand what it might be like for a child to access therapeutic support. I can still feel the overwhelming emotion I had from taking part in that exercise, the nervous energy, the apprehension, the fear all tinged with excitement. It was conflicting, overwhelming and powerful. This was me, living it through an exercise, this wasn’t the real thing. I wasn’t a child.
It is a normal response to be unsure about how to support your child in therapy; even if you have accessed support for yourself before. Being open and honest with your child is important as well as not asking questions of them; respecting their privacy and confidentiality. Remember, therapy is not ‘fun’; it may be play, and there may be elements of enjoyment, but it is therapy.
This guide seeks to provide you with some 12 pointers and ways in which you can support your child in getting the best out of the therapeutic process.
- Choosing the right therapist
This can be the most daunting part. Choosing the ‘right’ person for the job can be complex. The person who feels right, with the correct qualifications and professional registration is the person for the job. Don’t be afraid to ask questions of the therapist. The job you are asking them to do is very important and they need to be someone you can trust to support your child in their therapeutic journey.
Therapists on a professional register undergo checks to ensure they are adhering to codes of ethics and have the appropriate training. Have a read of our ‘Choosing a therapist’ post if you haven’t done so already.
2. Ensure your child knows what is happening
As a society we are getting better at being more direct with children in relation to mental health; but we still aren’t quite there. Mental health can be a difficult topic to navigate and you might not feel you have the right tools to answer all the questions. There are some great books to help you talk to your children about emotions and mental health such as My Hidden Chimp and What’s going on inside my head.
Be honest with your child, in an age appropriate way. It may be there is a clear trigger for the concerns; ie. A death in the family or parental separation or the concerns may be part of a longer term issue. When talking to your child about therapy, for younger children you might want to use phrases such as ‘things have been a bit tricky for you’, ‘I’ve noticed that sometimes your behaviour is telling me you are feeling angry/sad/worried’ or ‘when you do/say X I am wondering if you are feeling X/Y/Z’. Explain to them that you thought it would be helpful for them to see someone to think about their feelings, emotions or behaviours.
For older children you may be able to be more direct. You may, in a similar way, explain that you have noticed changes in their behaviour or mood, you may be able to tell them you are worried about them (if this is the case) and so you were wondering if they may want to speak to someone or see a therapist to think about how they are feeling and see if they can be supported.
Depending on the type of therapy you have chosen, explain to your child the support you are suggesting they access. If it is a non-directive (not necessarily needing words) therapy, let them know that they will not have to talk if they do not want to. For older children allowing them to choose the type of intervention can be helpful too.

3. Should I call it therapy?
Let’s be honest, it can feel uneasy saying your child is going to therapy. But who does this unease belong to. Is it your child’s? Probably not. It is most likely to be your unease in truth. Being an adult who has grown up in a society where mental health concerns are ‘hush hush’. Therapy is a word that has a lot of weight to it; but it is what it is, therapy. The stigma attached to the word is reducing and the way in which we do this is to be open and not suggesting it is shameful in anyway. My advice would be, to be honest. It is therapy. But it is also your choice what you call it – just don’t call it ‘fun time’.
4. Commit
This one is going to sound like a bit of a lecture; but it is important.
If you have decided your child needs therapy, and this requires you to take them to the sessions ie. it is not in school, commit to it. Your child is not able to get themselves to and from the therapy, and even if they can, support them emotionally by being there for them. Therapeutic input that is consistent is more effective. Be on time and attend all planned sessions. If for whatever reason there is going to be as session you can’t make for example a work meeting or a family holiday, let the therapist know in advance so they can work with your child with this in mind. The therapist may be able to make allowances for missed sessions, reschedule them etc. but this needs to be done in collaboration with you. Missing sessions or being late will impact on the effectiveness of the therapy. It is your child who will miss out.
Commit. Attend all planned sessions. Attend on time. Simple!
5. What will happen in the session?
This will vary from therapy to therapy. You should be invited by the therapist to meet with them before the first session. This should also happen if the therapy is due to happen in school. It is best if both you and your child have met the therapist prior to the intervention starting and have some idea of what the room will look like. It is okay to tell the child that you do not know what will happen if they ask and you are not sure. In the initial meeting some of these questions may get answered but more may arise. Assure your child it is okay to feel apprehensive. Support them in naming their feelings if they are expressing anxiety, worry, concern.
Support your child before this initial meeting to write down any questions they have. If they ask you something and you don’t know write it down and take it with you.
6. What should I do or say before the session?
As time goes on it is likely that this will feel less awkward. It is also likely that you are feeling awkward and not your child; older children may feel this more. You should have met with the therapist before-hand and so your child should have some idea of what to expect. As in point 4, support them in naming their feelings if they are appearing to be nervous, anxious, apprehensive for example.
Let them know that this is their time and you will not be asking question about their session. Remind them that you are there for them if they do want to share anything, but they do not have to.
7. What should I do after the session?
Sessions are confidential. If, as an adult, you were to go to a therapy session, you would not expect your friend or partner to ask ‘what did you talk about?’ when you get home and if they did, you would likely feel quite uneasy. Similarly, you would be unlikely to respond positively if you were asked ‘did you have fun?’ Please avoid asking your child if they had fun, what they did, what they talked about or if they are ‘okay’. It can be really difficult not to respond in this way to children. Think about what you naturally say to them when you pick them up from school or a club? That’s right, all of those phrases.
When you collect your child, simply be there for them. Greet them with a warm smile, nothing too forced, they may be feeling sad, allow them to have this feeling; don’t try to make them happy. Allow the emotion to be. A simple ‘Hello’ is enough. If they want to talk, they will. They may share, they may not.
I remember one of my clients who never spoke in her sessions and never shared with her mother what had happened in our work together, one day told her Mum about an event in the therapy room. This happened to be a really powerful point in her therapy. She had experienced domestic violence. In the session she had accidently spilt water and I did not shout. It was this she shared with her mother. It may not seem like a lot, but her mother being there, hearing her, not asking questions and just allowing the child to share the information was really helpful to the child.
If they talk, just listen. Do not be tempted to ask questions.
Therapy is a complex process. It can be tiring and is not always something that happens in the conscious. Perhaps take a snack and a drink for your child. Be prepared for their behaviour to perhaps be up and down for the next day or so. The therapist should give you an indication of any concerns that arose in the session; but they should not tell you about what happened in the session.
8. My child does not want to go!
Be prepared for your child to decide one week that they simply do not want to go to therapy. This is a very normal response, and although frustrating is part of the process for some children. They may be finding the processing too difficult in the room, they may be seeking to control when they feel out of control. Encourage your child to attend, but allow them to make the decisions. Let your child know that you are aware they are working hard in their sessions and you understand that it can be difficult to go to. Express that you understand that they want to stay and play on their tablet, but in the longer term going to see Sally the therapist will make things feel better for them. Remind them, in an age appropriate and gentle manner, of the reasons for the therapy.
Taking your child ‘kicking and screaming’ to the session is not going to be beneficial for anyone. If refusal to attend goes on, speak to your child’s therapist for support specific to your child.
9. When will things be better?
How long is a piece of string? This will vary from client to client and there may be some improvement and then things might seem to be more difficult again. Hold in there, stick with it, it will get better in time.
You should expect some disruption to behaviour and emotions following sessions and perhaps in the time leading up to the session too. As thoughts, feelings and emotions are processed this is reflected in behaviour. Acknowledge the difficulties. Behaviour which is dangerous will need consequences, but try to implement these when your child (and you!) is calm.
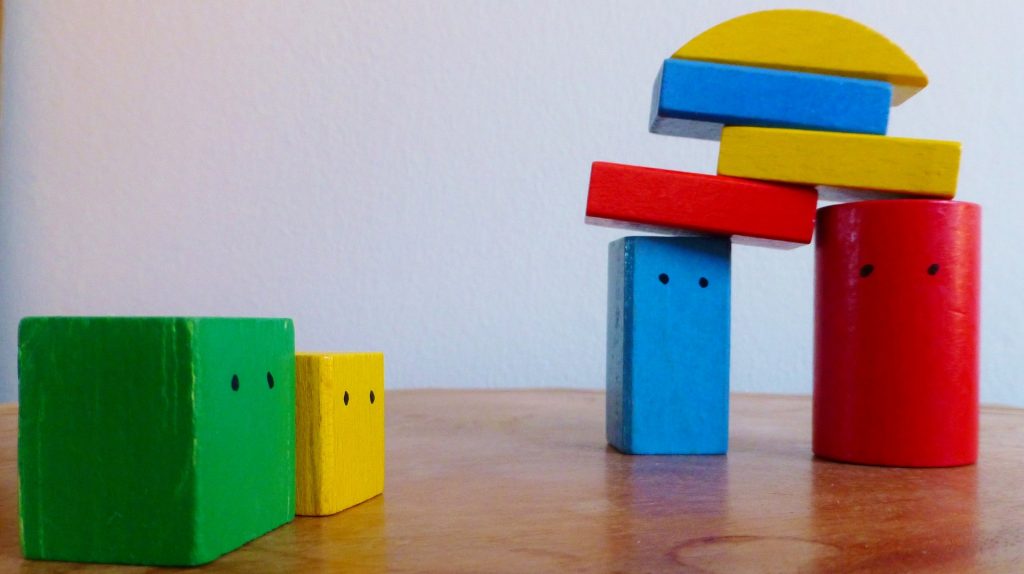
To illustrate this, if you think about feelings and emotions as building blocks; These blocks are perhaps not laid down solidly, they’re a bit wobbly for whatever reason. The therapy support takes these one by one and relays them, placing them on a more solid foundation. There is a settling period for these blocks, they may wriggle into their new setting to ensure their fit and as other events, emotions and feelings are processed and placed on top, these too will wriggle into place as well as the ones underneath ensuring their footing. This wriggling may be seen in expressed emotion or expressed through behaviour as sometimes words are too difficult to use.
10. What will the therapist tell me?
The therapist should share with you your children progress but not what is called the process. The process is what your child does in the room. What they say and do. The progress is the changes the therapist sees in the child. For example in play therapy, the therapist may observe your child engaging in a lot of conflict in their play. In time, hopefully, as is the aim of the therapy, this may reduce. The therapist may share with you that they have seen a reduction in the conflict seen in the play, for example.
The therapist should share no more than the progress your child is making. As much as if you went for personal therapy you would want the process to be confidential, your child should be afforded the same respect.
11. Should I tell my friends?
Whilst I advocate for therapy not to be a shameful experience and for it not to be hidden; I also advocate for the child to have the choice and for them to feel in control. This is their information, just because they are children, does not mean we have a right to share with everyone what they are experiencing.
That said, you may have a friend who you have been talking to about the difficulties you and your child have been facing. Before you share, think about why it is you are sharing the information. If it is to support you to support your child this would be more agreeable than chatting about it at the school gates.
12. Golden Rule: Do not refer to therapy as ‘fun’
I have mentioned this at a couple of other points in this post, but it really is key. Therapy is not ‘fun’. There may be elements of enjoyment and particularly if your child is engaging in something like play therapy, it may feel fun at times, but it is also a psychological process, one which can feel uncomfortable at times.
It is a bold brave step to take to start your child on the therapeutic process and it is brave of your child to attend. It’s not always an easy time. We hope that these pointers can help you in supporting your child with their therapeutic intervention. Your chosen therapist should also be able to answer any questions you may have specific to your child. If you do not have a therapist or have any other questions please contact us at Lily Pad Play Therapy and we will do our best to help.


Recent Comments